Tumor and Epilepsy Consortium: Featured Northeast Regional Epilepsy Program
Dr. Jeffrey Politsky is the Associate Director of the Northeast Regional Epilepsy Group in New Jersey, the Co-Director of Research and Medical Director of the MEG & Functional Brain Mapping Center of the Northeast Regional Epilepsy Group and the Atlantic Neuroscience Institute Epilepsy Center. One of his main clinical interests is epilepsy in tumor patients. He has been instrumental in fouding the tumor-related epilepsy research consortium which is growing into a multi-center, multi-national consortium that consists of a team of clinical experts, including epilepsy specialists, neurosurgeons, neuro-oncologists, and neuro-psychologists whose main interest is tumor-induced epilepsy. He sat with us to tell us more about epilepsy and brain tumors as well as future directions in this novel field.
1) How likely is it for someone to develop epilepsy with a brain tumor?
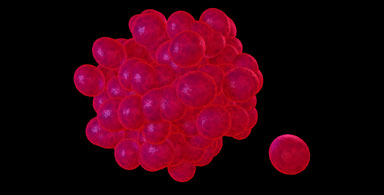
Approximately 40-60% of patients with brain tumors develop seizures. Some studies report the prevalence to be even higher. In most instances, the seizures are recurrent and the patient is described as having tumor-induced epilepsy (recurrent seizures).
2) What population is most at risk and what are other factors that may put people at risk?
The exact reasons why tumors cause epilepsy remain incompletely understood. The presence of a brain mass and the associated swelling, both of which put pressure on brain cells and pathways are not adequate explanations since these factors occur in almost every case but only a portion of patients develop epilepsy. Other relevant factors currently being studied include the tumor type (for example, intrinsic brain tumors like low or high grade gliomas, extrinsic brain tumors like meningiomas, or metastatic brain tumors that arise from a primary site outside the brain such as the lung, breast, or skin), tumor grade (how biologically active the tumor is), genetic alterations associated with tumor development, biologic substrates released and/or altered by the tumor, and sub-cellular damage and injury to name but some. There are other secondary causes of seizures in tumor patients, which relate to complications of treatment including chemotherapy, radiotherapy, surgery, immune suppression, and other metabolic conditions.
3) What are the symptoms that may point to a possible brain tumor in addition to seizures?
Overall, headaches are either the first or second most common symptom of a brain tumor other than seizures. Other symptoms, however, that may indicate a brain tumor or brain lesion is present really depend on the location of the tumor. A tumor in the motor or sensory area may cause weakness or a sensory disturbance. Changes in visual function including, hallucinations, visual loss, and/or double vision may be the symptom of a lesion behind the eye or in the occipital lobe at the back of the brain (occipital lobe). Changes in cognition (ability to think and/or remember), ability to speak or understand language may occur with lesions in the temporal lobe. Auditory hallucinations can also occur with lesions in the temporal lobe and other hearing problems may be the symptoms with lesions near the auditory canal. Personality changes can also be the primary symptom with lesions in the frontal lobes. And lesions in the brain stem may cause any or all of the above symptoms and as well as lethargy and coma, depending on the exact location and size of the lesion. Some tumors are more likely to rupture or bleed, which can cause sudden presentation of new symptoms or worsening of pre-existing symptoms.
4) Are there any preventative measures a person can take?
In many instances there are no preventative measures that a person can take to prevent the development of a brain tumor. Certain types of metastatic brain tumors are preventable: not smoking may prevent most types of lung cancer and protecting your skin may prevent development of melanoma, but most causes of cancer are not preventable. Regular check-ups and seeing a doctor if any new symptoms develop is the best way to identify a problem as early as possible. If your primary care doctor is concerned about any new symptoms, such as a headache, he or she should refer you to a neurologist. One of the doctors will likely order a CT scan (with contrast), which is a pretty good diagnostic tool to determine the presence or absence of a brain tumor. An MRI with gadolinium may also be recommended.
5) What are the treatment options available for people with epilepsy who have a brain tumor?
Treatments for patients with tumor induced epilepsy depend on the type of tumor. The mainstay of therapy is anti-seizure medications. Adjunctive treatments such as chemotherapy and radiotherapy may also be indicated for certain tumor types. Some very low-grade tumors cause refractory epilepsy and are easily treated by removing the tumor. Other tumors may also require surgery because of their type or grade. In many cases complete resection of the tumor is not possible because of its location. The treatment plan must be individualized for each patient.
6) Do you treat someone with a brain tumor who has epilepsy differently than someone who only has epilepsy alone?
A patient with tumor-induced epilepsy has two conditions: a brain tumor and epilepsy. Generally speaking, resecting the tumor only is a sufficient surgical procedure in someone with a brain tumor but without epilepsy. However, once a patient develops epilepsy, simply removing the tumor is not enough to cure the epilepsy. We are learning more and more about the interplay between tumors and epilepsy and the relationship is very complicated. A patient with tumor-induced epilepsy should be managed by a team that includes an epilepsy specialist, a neurosurgeon (preferably a functional neurosurgeon that deals with tumors and epilepsy), and a neuro-oncologist from the outset; many patients require functional cortical mapping, mapping of the epileptic network, and a surgical plan that aims to resolve both conditions. At the very least the patient should seek out a level IV epilepsy center.
7) Are there any medications that are indicated for epilepsy in a case that also has a tumor?
The anti-seizure medications used for patients with tumor-induced epilepsy are largely the same for patients with refractory epilepsy. There is some limited evidence that some anti-seizure medications may work better for tumor-induced epilepsy compared with non-tumor-induced epilepsy because of the concentration the drug achieves in the brain, or because the drug may also inhibit tumor growth. This is an area of expanding research.
8) What other diagnostic tools are helpful in patients with brain tumors?
Other than CT and MRI scans, VEEG is very important because this can help determine if a patient is at risk for having seizures even if the patient has never had one by analyzing the brain's electrical impulses. A Magnetoencephalogram (MEG) can provide a similar answer by measuring the magnetic impulses generated by an electrical impulse: MEG and VEEG are complementary. MEG can also assess cortical function. But still, patients with lesions in eloquent brain areas (see 2 above) will likely require bedside or intraoperative functional cortical mapping. And finally, a PET scan may help by showing focal metabolic changes caused by a tumor.
9) How does your program help those with epilepsy and brain tumors?
Our program has a team of epilepsy fellowship trained and board certified adult and pediatric neurologists that work in concert with the other specialists necessary for successful management of this complicated subset of patients regardless of age: that is both pediatric and adult patients. We have several Level IV epilepsy centers in NJ and NY.
10) What is the tumor consortium that you, Dr. Politsky and the Northeast Regional Epilepsy Group are working on?
The tumor-related epilepsy research consortium was founded this past year and is growing into a multi-center, multi-national consortium that consists of a team of clinical experts, including epilepsy specialists, neurosurgeons, neuro-oncologists, and neuro-psychologists whose main interest is tumor-induced epilepsy. For far too long, patients with brain tumors who developed seizures were given an anti-seizure medication with no further attention paid to the epilepsy. We are now learning that these are two dynamic processes or conditions that each can influence the outcome of the other. The Northeast Regional Epilepsy Group is playing a critical role by supporting the development of the infrastructure of this consortium. I am dedicating my time to facilitate the development of this consortium because I am very interested in the field and because t is a much-needed initiative that I hope will pay dividends in the form of prolonging and improving quality of life for the scores of patients with tumor-induced epilepsy. Soon we will have a website and a blog
